Who Can Read a Cervical Spine M R I
 We've previously published a weblog on the lumbar spine years ago. "Understanding your MRI of the Lumbar Spine". The cervical sequel is tardily but at to the lowest degree information technology showed up to the party.
We've previously published a weblog on the lumbar spine years ago. "Understanding your MRI of the Lumbar Spine". The cervical sequel is tardily but at to the lowest degree information technology showed up to the party.
Cervical spine arthritic degeneration results from increased mechanical stressors passing through the cervical spinal column, resulting in bone spur formation (uncovertebral spurring) and secondary degenerative changes in surrounding structures. This includes loss of top and water content in the discs, and enlargement of the facet joints and ligaments. Prove of these degenerative changes are even found in asymptomatic adults, including 25% under the age of forty, 50% over the age of 40, and 85% over the age of 60. The most common show of degeneration is found at C5-6 followed past C6-vii and C4-5, as these levels are the most naturally mobile in the cervix.
That'south right, as we all get into our xx's, our cervical and lumbar spine starts to develop arthritis. This isn't a disease simply for your grandparents. While modern medicine fixes many problems, our bodies simply weren't made to live this long. King Tut died around the age of nineteen, which was common in that era, however those Egyptian spines weren't evolutionarily much different than ours today.
Fortunately, many people are completely asymptomatic. Unfortunately, others can develop neck hurting, regional shoulder pain, or develop neurologic deficits from pressure on the spinal cord and/or nerves.
Cervical spine degeneration tin be mistaken with other weather, like muscle strains or shoulder problems. Not every patient experiences the same symptoms or signs, and then evaluating your individual status may all-time be accomplished by talking to a specialist, and non just comparison complaints with a friend or family.
Just as is the depression back, most people (approximately 70%) become ameliorate with simply residual, time and over-the-counter medications. If afterward four to half dozen weeks of symptoms without improvement, some therapy or basic imaging, like an 10-ray, may be beneficial.
Advanced imaging, like a cervical MRI, is reasonable when symptoms have been persistent after well-nigh half dozen weeks of conservative management, or there is an aberrant neurologic examination suggesting nerve compression.
Information technology's pretty mutual nowadays for patients to receive their MRI report and nearly people read these reports and try to empathize what is wrong. With the ease of internet access, cocky-diagnosis is very common, but there'southward a reason Google is free and a medical educational activity is hundreds of thousands of dollars. What's important to remember is that the report is made by a radiologist (a medico specifically trained to review these images) who must study everything they encounter. At present radiologists may miss sure findings too, while doing their all-time. But the radiologist makes this written report often without any consideration of patient's symptoms. This is why, ordinarily, radiologists are not the physicians calling patients about their written report. Therefore the MRI may mention many different findings or abnormalities, making patients feel like everything is incorrect with their spine. Withal all, none or some of these findings may explain the symptoms. Additionally, the severity of findings is very subjective and may vary between unlike physicians or radiologists. What is "severe" to one physician, may not appear so bad to another. It's imperative that you discuss the MRI study with a spine specialist to see which, if whatever, of these findings are important and demand to be addressed. The spine specialist should review the actual images with yous and reply any questions yous accept about your written report. If surgery eventually is required, surgery is intended to just gear up the problems causing the symptoms and not to make your spine or MRI look perfect.
Normal Anatomy of the Cervical Spine
Earlier deciphering the abnormalities listed in the cervical MRI report, it'southward important to understand the normal anatomy.
The cervical spine consists of basic (commonly 7 vertebral bodies) stacked on height of each other and separated by 6 discs. In that location is no disc between the first and 2d cervical vertebrae. The vertebral bodies are normally labeled 1 through 7, and the discs are named by the basic to a higher place and below. Therefore the C4 and C5 vertebral bodies are separated by the C4-5 disc. The back side of the spine is more os called the lamina and spinous process. This normal configuration is reported in the MRI written report as both sagittal and axial depictions. The sagittal view is a profile motion picture. The centric view is a cross-section.
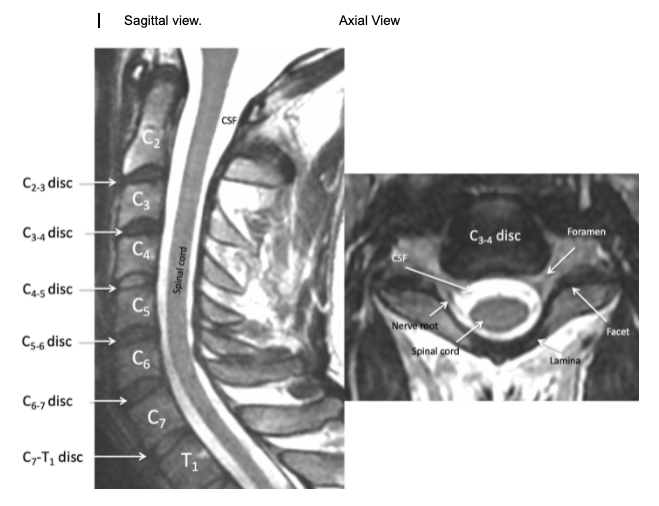

The viewpoint is similar to the lumbar spine.
Just behind the column of bones and discs is the sac which holds the spinal string, nerve roots and fluid, called cerebral spinal fluid (CSF). At present this is dissimilar from the lumbar spine. The spinal cord itself, which is considered part of the "key nervous organisation" and cannot necessary be repaired if injured, spans from the brain to the ~ T12 or L1 or L2 level. Therefore the cervical spine encases the spinal string, whereas most of the lumbar spine encases peripheral spinal fretfulness, called the cauda equina.
![]()
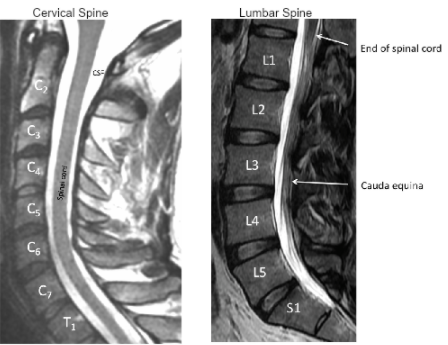
The normal cervical spine culvert should be between 10-14 millimeters. Some study fifty-fifty larger, upwards to 16 millimeters. Sometimes this measurement is included in a report. The spinal cord itself extends through the entire cervical spine. At each disc level, a nerve exits the spine and goes to a specific region of the arm.
![]()
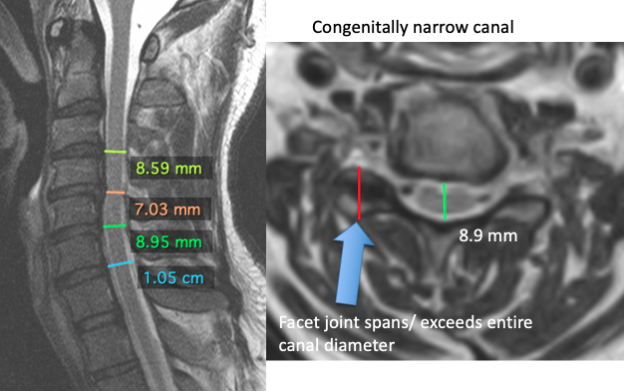
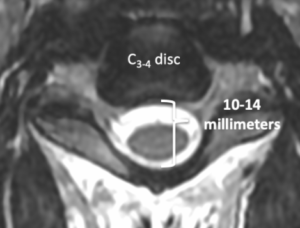
Some patients are born with smaller-than-normal cervical canals. This is termed a, "congenitally narrow canal" or "congenital stenosis". Often, congenital stenosis can be speedily recognized when the facets centric length spans or exceeds the sagittal diameter of the canal. With a "smaller" canal at baseline, these patients may exist more than susceptible to spinal cord compression with more than minimal changes in the discs, bone spurs or ligaments, than one with a more than standard canal. However congenital narrowing may also be a finding without whatsoever clinical significance. This does not hateful any intervention is required.
![]()
Pressure on the spinal cord itself may cause symptoms in the arms or legs considering all the nerves heading to the lumbar spine have to pass through the cervical spine first. Nonetheless the nerve roots become to specific regions of simply the arms. A cervical nervus root compression would not explicate leg symptoms. The C5 nervus tends to become the shoulder, or deltoid muscle. The C6 to the bicep. The C7 to the tricep. The C8 and T1 usually to the hand. In that location is also a co-operative of the cervical nerve that extends to the muscles between the shoulder blades. Spasm in the interscapular region sometimes originate from the neck, but are mistaken to experience like a problem with the thoracic spine.
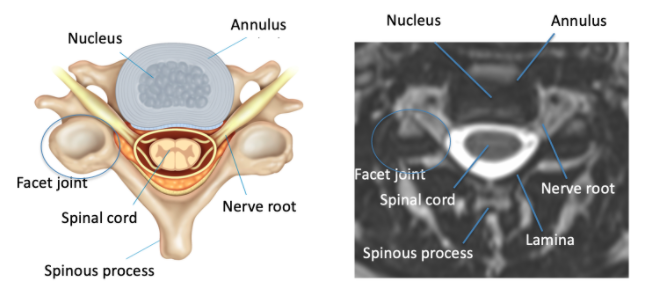
Just as in the lumbar spine, the cervical disc is equanimous of two parts. These are microscopic and cannot exactly be differentiated on an MRI. The central softer part of the disc is the nucleus and the out layer is the annulus. Normally, the annulus holds the nucleus in the center and there is no contact with the nerve roots.
Problems in the Cervical Spine
As we get older, changes occur naturally in the spine. The discs tend to lose their h2o content (desiccate). The annulus of the disc may burl, protrude or extrude/ herniate. The bones may develop bone spurs (osteophytes). The ligamentum flavum may enlarge (hypertrophy). The facet joints may enlarge (hypertrophy). The joints attached to the vertebral body (uncovertebral joints/ Luschka joints) may enlarge The bones may slip on one another (subluxation or spondylolisthesis). The outcome of these changes may narrow the place where the nerve exits the spine (foraminal stenosis). These changes may narrow the canal where the spinal cord resides in the spine (cardinal stenosis). Each of these things may happen and not cause whatsoever symptoms. On the other hand, these problems may start pressing on the spinal cord/ nerves causing pain, weakness, numbness, balance problems or "myelopathy". Listed are some unremarkably occurring changes, which may be described in a cervical MRI written report. The nigh mutual levels affected at C4-v, C5-half-dozen and C6-7 equally these are the most mobile levels in the cervical spine.
Cervical Spondylosis
This term is very broad and can be used to describe any arthritis in the cervical spine.
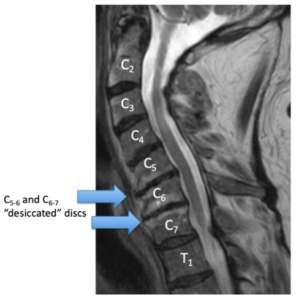 Disc Desiccation
Disc Desiccation
Besides called "loss of disc pinnacle" or "night discs". Disc desiccation is a nonspecific term which describes natural "aging" of the discs. When we are young, the discs take a lot of h2o or cushioning in them. Every bit we get older, the disc naturally loses its water and essentially shrinks. This can lead to "narrowing of the disc infinite", "disc flattening" or "bone on bone" changes, however, this occurs in every person and this is non necessarily a crusade of any symptoms.
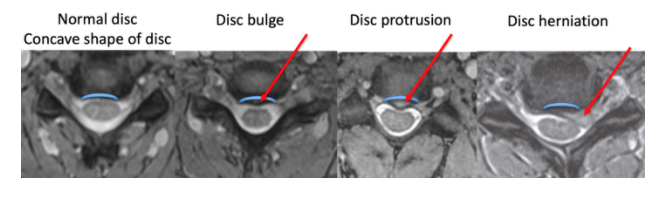
Disc Burl/ Disc Protrusion/ Disc Extrusion or Herniation etc…
These terms are variations of the same concept. A normal cervical disc has a shine concave (arch) shape over the spinal canal. Typically a bulge simply means the annulus is weaker and deviates towards the nerve sac. Bulges are extremely common and rarely cause whatsoever hurting or symptoms. Many people take them at multiple levels in their spine. Protrusion is a slight progression in which the disc now MAY focally straight towards the cord or nerve. An extrusion or herniation occurs when a piece of the nucleus now has exited the disc and is possibly pressing on a nerve or the spinal cord.
Information technology is difficult to understand, just the coverings of the spinal fretfulness (dura) have minimal pain receptors. The spinal cord itself too lacks hurting receptors. It'due south the part of the cervical spinal nerve, chosen the dorsal root ganglion, which typically mediates pain. What this insinuates is that central disc bulges, protrusions, or even herniations, oftentimes may non cause pain. This is true even when the bulge, protrusion, or even herniation may deform the cord or its sac. It normally is when the herniation, bone spur, or facet compresses the nerve root's dorsal ganglion when pain symptoms develop.
At that place is also a sequence on cervical MRI, called the slope repeat, which tin can help your treating provider know if the herniation is new or old. Newer disc changes appear whiter while chronic announced darker.
 Osteophytes
Osteophytes
Also chosen "os spurs." Osteophytes are bony changes that occur with natural aging. They are commonly associated with other findings such every bit disc bulges. The bony edges, that attach to the discs, can enlarge as the discs burl and may or may not compress the nerves. This is commonly referred to as "uncovertebral hypertrophy" Merely as with disc bulges, these are very common. All the same if the uncovertebral hypertrophy is meaning plenty, information technology could compress the nerves and cause symptoms.
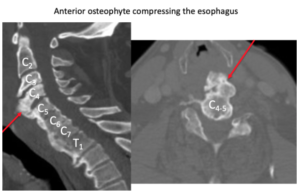
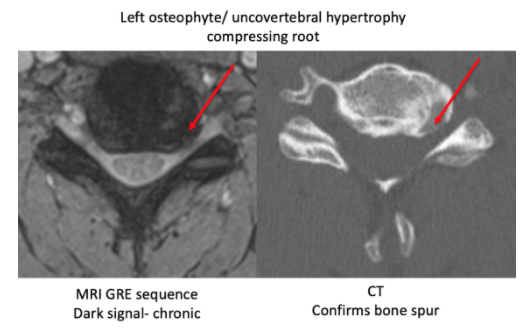 In the cervical spine, inductive osteophytes may likewise occur. Every bit these bone spurs course in front of the spine, they will not printing on any fretfulness or crusade neurologic bug. Withal in very rare cases, they may become then large they could shrink the esophagus and crusade swallowing problems.
In the cervical spine, inductive osteophytes may likewise occur. Every bit these bone spurs course in front of the spine, they will not printing on any fretfulness or crusade neurologic bug. Withal in very rare cases, they may become then large they could shrink the esophagus and crusade swallowing problems.
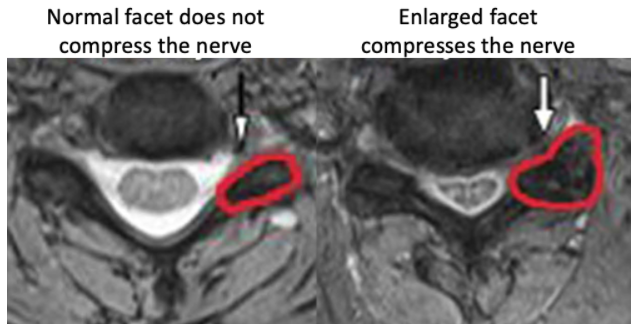
 Facet Hypertrophy
Facet Hypertrophy
The facets are the joints in the back that help the spine movement. The spine is substantially a 3-legged tabular array. The disc is the largest leg in the front. The 2 facets are the 2 back legs.
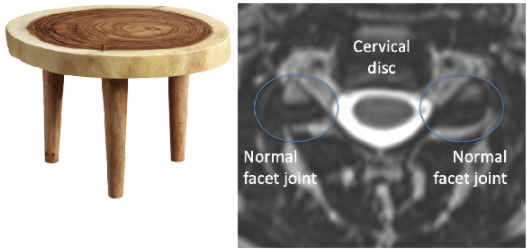
As we historic period, the facets tin can become larger and may, or may not, press into the fretfulness. This may, or may not, cause pain in the neck or arms.
![]()
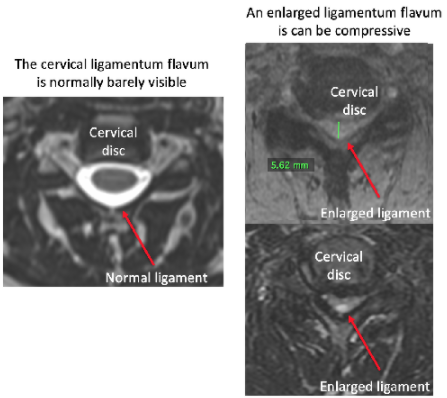 Ligamentum Hypertrophy
Ligamentum Hypertrophy
The ligamentum flavum is a tissue only backside the nervus sac. Equally we age, this ligament can get bigger or hypertrophy. Depending on how much information technology enlarges, it could press on the nerves and potentially crusade symptoms. Usually, the ligamentum hypertrophies in combination with a disc bulge.
![]()
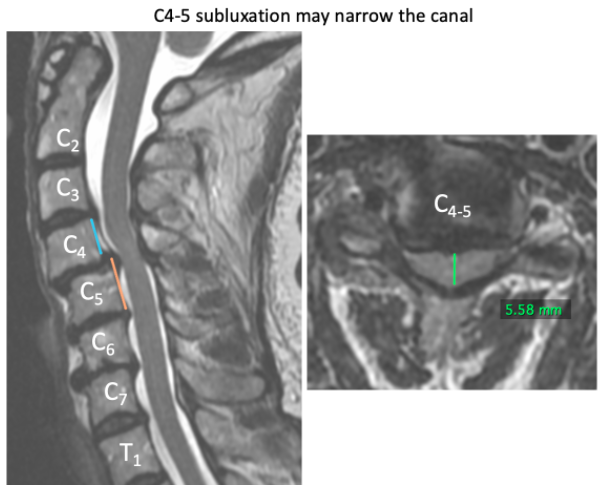
Spondylolisthesis/ Subluxation
These ii terms refer to the vertebral bodies slipping over ane some other. Everywhere in the spine the basic should exist aligned. As we historic period, the ligaments holding the bones in place can loosen and allow the basic to sideslip. This tin can too occur from a fracture. In either case, this condition may or may not be symptomatic.
![]()
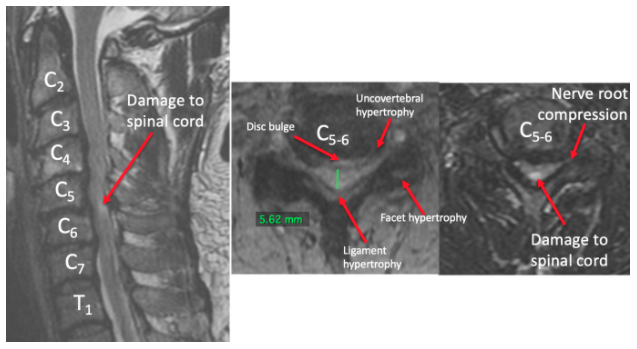 Stenosis
Stenosis
Stenosis refers to a situation in which a space is made smaller. Information technology's a very general term. The central canal, where the spinal cord resides, tin can go smaller, causing central stenosis. The foramen where the nerves exit the spine can become smaller, causing foraminal stenosis. Anything from a disc bulge to an osteophyte to ligamentum hypertrophy to facet hypertrophy to spondylolisthesis tin cause key or foraminal stenosis. Whether or not this causes symptoms depends on the degree of stenosis and if the stenosis is causing inflammation of the nerves. Surprisingly, severe central or foraminal stenosis tin be asymptomatic, if inflammation does not follow.
![]()
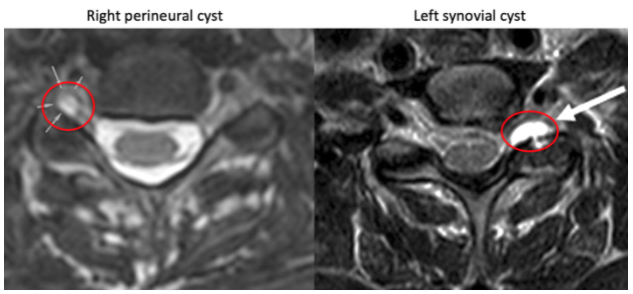 Cysts
Cysts
Cysts may form around the cervical nerve roots. These are typically chosen "perineural cysts". These are adequately common and do non appear to cause symptoms.
On the other hand, cysts may form from the facet articulation, chosen "synovial cysts". These may be compressive and could crusade symptoms.
![]()
Symptoms
In summary, the MRI findings do not determine whether or not symptoms are occurring. A person's MRI can appear fairly normal and they can be in terrible pain with many symptoms. On the other manus, a person can exist asymptomatic with an MRI showing awful disc extrusion, hypertrophies and spondylolisthesis. The way we accurately treat patients is past correlating their symptoms to specific changes in their MRI. The puzzle pieces must fit together.
It is imperative that the patient understands the cause of their symptoms and the treatment options. If you take an MRI showing changes, information technology is recommended yous meet with a spine specialist to encounter if these changes can explain your symptoms. If it does not appear they explain your clinical moving-picture show, that does not mean you are crazy or anyone is questioning your hurting. There are many causes for neck and arm symptoms, and only some are explained by a cervical spine structural change.
Source: https://rockymountainbrainandspineinstitute.com/understanding-your-cervical-mri/
0 Response to "Who Can Read a Cervical Spine M R I"
إرسال تعليق